
MIPS Seminar Series: “Convergent, translational research to improve human health”
Joseph M. DeSimone, PhD
Sanjiv Sam Gambhir Professor of Translational Medicine and Chemical Engineering
Departments of Radiology and Chemical Engineering
Graduate School of Business (by Courtesy)
Stanford University
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/98460805010
Dial: +1 650 724 9799 or +1 833 302 1536
Webinar ID: 984 6080 5010
Passcode: 809226
12:00pm – 12:45pm Seminar & Discussion
RSVP Here
ABSTRACT
In many ways, manufacturing processes define what’s possible in society. Central to our interests in the DeSimone laboratory are opportunities to make things using cutting-edge fabrication technologies that can improve human health. This lecture will describe advances in nano- / micro-fabrication and 3D printing technologies that we have made and employed toward this end. Using novel perfluoropolyether materials synthesized in our lab in 2004, we invented the Particle Replication in Non-wetting Templates (PRINT) technology, a high-resolution imprint lithography-based process to fabricate nano- and micro-particles with precise and independent control over particle parameters (e.g. size, shape, modulus, composition, charge, surface chemistry). PRINT brought the precision and uniformity associated with computer industry manufacturing technologies to medicine, resulting in the launch of Liquidia Technologies (NASDAQ: LQDA) and opening new research paths, including to elucidate the influence of specific particle parameters in biological systems (Proc. Natl. Acad. Sci. USA 2008), and to reveal insights to inform the design of vaccines (J. Control. Release 2018), targeted therapeutics (Nano Letters 2015), and even synthetic blood (PNAS 2011). In 2015, we reported the invention of the Continuous Liquid Interface Production (CLIP) 3D printing technology (Science 2015), which overcame major fundamental limitations in polymer 3D printing—slowness, a very limited range of materials, and an inability to create parts with the mechanical and thermal properties needed for widespread, durable utility. By rethinking the physics and chemistry of 3D printing, we created CLIP to eliminate layer-by-layer fabrication altogether. A rapid, continuous process, CLIP generates production-grade parts and is now transforming how products are manufactured in industries including automotive, footwear, and medicine. For example, to help address shortages, CLIP recently enabled a new nasopharyngeal swab for COVID-19 diagnostic testing to go from concept to market in just 20 days, followed by a 400-patient clinical trial at Stanford. Academic laboratories are also using CLIP to pursue new medical device possibilities, including geometrically complex IVRs to optimize drug delivery and implantable chemotherapy absorbers to limit toxic side effects. Vast opportunities exist to use CLIP to pursue next-generation medical devices and prostheses. Moreover, CLIP can improve current approaches; for example, the fabrication of an iontophoretic device we invented several years ago (Sci. Transl. Med. 2015) to drive chemotherapeutics directly into hard-to-reach solid tumors is now being optimized for clinical trials with CLIP. New design opportunities also exist in early detection, for example to improve specimen collection, device performance (e.g. microfluidics, cell sorting, supporting growth and studies with human organoids), and imaging (e.g. PET detectors, ultrasound transducers). Here at Stanford, we are pursuing new 3D printing advances, including software treatment planning for digital therapeutic devices in pediatric medicine, as well as the design of a high-resolution printer capable of single-digit micron resolution to advance microneedle designs as a potent delivery platform for vaccines. The impact of our work on human health ultimately relies on our ability to enable a convergent research program to take shape that allows for new connections to be made among traditionally disparate disciplines and concepts, and to ensure that we maintain a consistent focus on the translational potential of our discoveries and advances.
ABOUT
Joseph M. DeSimone is the Sanjiv Sam Gambhir Professor of Translational Medicine and Chemical Engineering at Stanford University. He holds appointments in the Departments of Radiology and Chemical Engineering with a courtesy appointment in Stanford’s Graduate School of Business. Previously, DeSimone was a professor of chemistry at the University of North Carolina at Chapel Hill and of chemical engineering at North Carolina State University. He is also Co-founder, Board Chair, and former CEO (2014 – 2019) of the additive manufacturing company, Carbon.
DeSimone is responsible for numerous breakthroughs in his career in areas including green chemistry, medical devices, nanomedicine, and 3D printing, also co-founding several companies based on his research. He has published over 350 scientific articles and is a named inventor on over 200 issued patents. Additionally, he has mentored 80 students through Ph.D. completion in his career, half of whom are women and members of underrepresented groups in STEM. In 2016 DeSimone was recognized by President Barack Obama with the National Medal of Technology and Innovation, the highest U.S. honor for achievement and leadership in advancing technological progress. He is also one of only 25 individuals elected to all three branches of the U.S. National Academies (Sciences, Medicine, Engineering). DeSimone received his B.S. in Chemistry in 1986 from Ursinus College and his Ph.D. in Chemistry in 1990 from Virginia Tech.
Hosted by: Katherine Ferrara, PhD
Sponsored by: Molecular Imaging Program at Stanford & the Department of Radiology

CEDSS: Disseminated cell hybrids as biomarkers for cancer detection, prognosis and treatment response
Melissa Wong, Ph.D.
Associate Professor and Vice Chair
Department of Cell, Development and Cancer Biology
Program Co-Lead, Knight Cancer Institute
Oregon Health & Science University
Zoom Details
Meeting URL: https://stanford.zoom.us/s/98184098662
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Meeting ID: 981 8409 8662
Passcode: 084321
ABSTRACT
Metastatic progression defines the final stages of tumor evolution and underlies the majority of cancer-related deaths. The heterogeneity in disseminated tumor cell populations capable of seeding and growing in distant organ sites contributes to the development of treatment resistant disease. We recently reported the identification of a novel tumor-derived cell population, circulating hybrid cells (CHCs), harboring attributes from both macrophages and neoplastic cells, including functional characteristics important to metastatic spread. These disseminated hybrids outnumber conventionally defined circulating tumor cells (CTCs) in cancer patients. It is unknown if CHCs represent a generalized cancer mechanism for cell dissemination, or if this population is relevant to the metastatic cascade. We detect CHCs in the peripheral blood of patients with cancer in myriad disease sites encompassing epithelial and non-epithelial malignancies. Further, we demonstrate that in vivo-derived hybrid cells harbor tumor-initiating capacity in murine cancer models and that CHCs from human breast cancer patients express stem cell antigens, features consistent with the ability to seed and grow at metastatic sites. We reveal heterogeneity of CHC phenotypes reflect key tumor features, including oncogenic mutations and functional protein expression. Importantly, this novel population of disseminated neoplastic cells opens a new area in cancer biology and renewed opportunity for battling metastatic disease.
ABOUT
The research focus of the Wong laboratory revolves around understanding the regulatory mechanisms that control epithelial stem cell homeostasis and their expansion in developmental, homeostasis and disease contexts, including cancer. I have substantial training and experience in intestinal stem cell investigation leveraging in vivo and ex vivo modeling, as well as in myriad cutting edge technologies (i.e. cyCIF, scRNA-seq). My publication record spans my post-doctoral fellowship in Dr. Jeffrey Gordon’s laboratory at Washington University School of Medicine, to studies in my own laboratory at Oregon Health & Science University. Our research impacts the understanding of regulatory mechanisms that govern cell state in the context of the evolving tissue microenvironment and changing cell signaling landscape, in development and disease.
Our studies in stem cell regulation led to the intriguing finding that stem cells can fuse with tissue macrophages in the context of injury repair and may impact tissue regeneration. We have extended these findings to the cancer setting, where cancer-macrophage fusions are detectible in primary and metastatic tumors, and my group recently identified and characterized these cells as a novel circulating tumor cell population. Importantly, our studies in cell culture, in mice and humans provide an indepth evaluation of hybrid cells to set the foundation for continued investigations into their biology, impact on disease progression or tissue regeneration, and use as a biomarker for disease burden. Importantly, we coined the term, circulating hybrid cell (CHC) for this novel population and reported they exist at higher levels than conventionally defined circulating tumor cells in the peripheral blood of cancer patients. This work was published in 2018 and highlighted by Science Magazine as one of the top ten publications in the cancer field in the science family journals. The science proposed in this U01 application leverage hybrid cell biology to assess treatment response and resistance in breast cancer patients undergoing targeted therapy. Our proposal leverages active collaborations with Dr. Young Hwan Young’s group to synergize biology with computation, as well as a number of other valuable collaborators to ensure success of the proposed, cutting-edge science.
Hosted by: Utkan Demirci, Ph.D.
Sponsored by: The Canary Center & the Department of Radiology
Stanford University – School of Medicine


Geert Litjens, PhD
Assistant Professor in Computational Pathology
Department of Pathology
Radboud University Medical Center
Title: Going Beyond What is Humanly Possible: Machine Learning for Clinical Pathology
Abstract: Machine learning advances in the past decade have revolutionized computer vision, and have since also made their way into medical imaging. Although many associate medical imaging with radiology first, clinical pathology might be more significantly impacted, at least in the short term by machine learning. Partly due to the simultaneous advent of machine learning in medicine and digital pathology, but perhaps mostly because in pathology achieving inhuman feats is surprisingly low-hanging fruit. In this presentation, I will give some examples analog to radiology, then illustrate some superhuman applications. Subsequently, I will highlight our current limitations and possible future research directions.
Radiology Department-Wide Research Meeting
• Dominik Fleischmann, MD: 3DQ Lab Overview
• Tom Soh, PhD: Research Updates
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

Join us for the annual Precision Health & Integrated Diagnostics Symposium. This all-day virtual event will showcase the exciting PHIND work that is going on campus wide. The featured presentations will be from current PHIND investigators and Precision Health experts. We hope you can join us and look forward to building the PHIND community together.
The agenda and speaker information are available on the PHIND website. The event is fully virtual and the livestream link will be posted on the PHIND website closer to the event.

MIPS Seminar Series: “Circulating Tumor DNA Biomarkers for Therapy Monitoring and Early Detection”
Shan X. Wang, PhD
Leland T. Edwards Professor in the School of Engineering
Professor of Materials Science & Engineering, jointly of Electrical Engineering, and by courtesy of Radiology (Stanford School of Medicine)
Director, Stanford Center for Magnetic Nanotechnology
Stanford University
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/93202777468
Dial: +1 650 724 9799 or +1 833 302 1536
Webinar ID: 932 0277 7468
Passcode: 851144
12:00pm – 12:45pm Seminar & Discussion
RSVP Here
ABSTRACT
Inspired by Dr Sam Gambhir, MIPS, Canary Center, and Stanford CCNE have pursued in vivo imaging and in vitro diagnostic tests for cancer therapeutic response or early detection, respectively, over the last 15+ years. Here I present two successful examples based on circulating tumor DNA (ctDNA) targets in plasma, complementary to imaging modalities such as CT and Ultrasound.
We have developed a simple yet highly sensitive assay for the detection of actionable mutational targets such as Epidermal Growth Factor Receptor (EGFR) and Kirsten rat sarcoma oncogene (KRAS) mutations in the plasma ctDNA from non-small cell lung cancer (NSCLC) patients using giant magnetoresistive (GMR) nanosensors. Our assay achieves lower limits of detection compared to standard fluorescent PCR based assays, and comparable performance to digital PCR methods. In 30 patients with metastatic disease and known EGFR mutation status at diagnosis, our assay achieved 87.5% sensitivity for Exon19 deletion and 90% sensitivity for L858R mutation while retaining 100% specificity; additionally, our assay detected secondary T790M mutation resistance with 96.3% specificity while retaining 100% sensitivity. We re-sampled 13 patients undergoing tyrosine kinase inhibitor (TKI) therapy 2 weeks after initiation to assess response, our GMR assay was 100% accurate in correlation with longitudinal clinical outcome, and the responders identified by the GMR assay had significantly improved progression free survival (PFS) compared to the non-responders. The GMR assay is low cost, rapid, and portable, making it ideal for detecting actionable mutations at diagnosis and non-invasively monitoring treatment response in the clinic.
On another front, we have also developed a highly sensitive and multiplexed assay for the detection of methylated ctDNA targets in plasma samples. Current diagnostic tests for liver cancer in at-risk patients are cumbersome, costly and inaccurate, resulting in a need for accurate blood-based tests. By devising a Layered Analysis of Methylated Biomarkers (LAMB) from the relevant big data, we have discovered a set of DNA targets in the blood that accurately detects liver cancer in these at-risk patients. This set of methylated targets was found by analyzing the genetic information of 3411 liver cancer patients and 1722 healthy people. Our results could lead to clinical adoption of liquid biopsy tests for liver cancer surveillance in high-risk populations and the development of blood tests for other cancers.
ABOUT
Prof. Wang directs the Center for Magnetic Nanotechnology and is a leading expert in biosensors, information storage and spintronics. His research and inventions span across a variety of areas including magnetic biochips, in vitro diagnostics, cancer biomarkers, magnetic nanoparticles, magnetic sensors, magnetoresistive random access memory, and magnetic integrated inductors. He has over 300 publications, and holds 65 issued or pending patents in these and interdisciplinary areas. He was named an inaugural Fred Terman Fellow, and was elected a Fellow of the Institute of Electrical and Electronics Engineers (IEEE) and a Fellow of American Physical Society (APS) for his seminal contributions to magnetic materials and nanosensors. His team won the Grand Challenge Exploration Award from Gates Foundation (2010), the XCHALLENGE Distinguished Award (2014), and the Bold Epic Innovator Award from the XPRIZE Foundation (2017).
Dr. Wang cofounded three high-tech startups in Silicon Valley, including MagArray, Inc. and Flux Biosciences, Inc. In 2018 MagArray launched a first of its kind lung cancer early diagnostic assay based on protein cancer biomarkers and support vector machine (SVM). In 2019, Flux Biosciences launched a human trial to offer at-home testing of fertility based on hormones and magneto-nanosensors. Through his participation in the Center for Cancer Nanotechnology Excellence (as co-PI of the CCNE) and the Joint University Microelectronics Program (JUMP), he is actively engaged in the transformative research of healthcare and is developing emerging memories for energy efficient computing.
Hosted by: Katherine Ferrara, PhD
Sponsored by: Molecular Imaging Program at Stanford & the Department of Radiology

Mixed Reality for Surgical Guidance will take place on Thursday, April 1st from 9:00 – 10:30 am PDT.
The event will start with a one-hour panel discussion featuring Dr. Bruce Daniel of Stanford Radiology and the Stanford IMMERS Lab; Christoffer Hamilton of Brainlab, a surgical software and hardware leader in Germany; and Dr. Thomas Grégory of Orthopedic Surgery at the Université Sorbonne Paris Nord.
This panel will be moderated by Dr. Christoph Leuze of Stanford University and the Stanford Medical Mixed Reality (SMMR) program.
Immediately following the panel discussion, you are also invited to a 30-minute interactive session with the panelists where questions and ideas can be explored in real time.
Register here: https://stanford.zoom.us/meeting/register/tJcqf-GrqToiHNKL4D-5haRLowQylIwMEAve

Date: April 10, 2021 (8 AM-6PM)
-
- 8 AM-8:20 AM opening remarks Zainub and Pete
- 8:20 AM-9:20 AM Talk 1 “I fought the law and no one won”
- 10 minute Break
- 9:30 AM-10:30 AM talk 2 students and doctors with disabilities panel
- 20 minute break
-
- 10:50 AM-11:50 AM Breakout
- One hour lunch (TBD)
- 12:50 PM-1:50 PM Talk 3 the frontiers of disability research
- Lisa Meeks is moderating
- Bonnie Swenor invited
- 10 minute break
- 2:00 PM-3:00 PM breakout 2
- 10 minute break
- 3:10 PM-4:10 PM talk 4 do-it-yourself disability advocacy (Poullos/Tolchin with students)
- 4:10 PM-4:30 PM closing remarks
- 4:30 PM-6 PM virtual happy hour

Radiology Department-Wide Research Meeting
• Research Announcements
• Michelle James, PhD – Detecting and Tracking Immune Responses in the Brain and Beyond using PET
• Ryan Spitler, PhD – Precision Health and Integrated Diagnostics (PHIND) Center
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

PHIND Seminar Series: Impact of the Veterans Affairs National Abdominal Aortic Screening Program
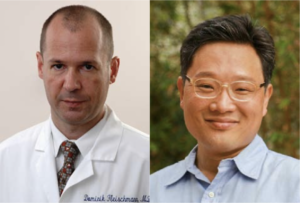
Manuel Garcia-Toca, M.D.
Clinical Professor of Surgery
Chief, Division of Vascular Surgery
Santa Clara Valley Medical Center (SCVMC)
Oliver O. Aalami, M.D.
Clinical Associate Professor of Surgery, Vascular Surgery
Lucile Packard Children’s Hospital
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/98417624095
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Webinar ID: 984 1762 4095
Passcode: 111283
11:00am – 12:00pm Seminar & Discussion
RSVP Here
ABSTRACT
Background: The U.S. Federal Government enacted the Screen for Abdominal Aortic Aneurysms Very Efficiently Act in January 2007. Simultaneously, the Department of Veterans Affairs (VA) implemented a more inclusive AAA screening policy for veteran beneficiaries shortly afterwards.
Our study aimed to evaluate the impact of the VA program on AAA detection rate and all-cause mortality compared to a cohort of patients whose aneurysms were identified by other abdominal imaging.
Methods: We identified veterans with an AAA screening study using the two existing Current Procedural Terminology (CPT) codes (G0389 and 76706). In the comparison group, eligible abdominal imaging studies included ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) queried according to CPT codes between 2001 and 2018.
We used a difference-in-differences regression model to evaluate the change in aneurysm detection rate and all-cause mortality five years before and eleven years after the VA implemented the screening policy in 2007.
We calculated survival estimates after AAA screening or non-screening imaging of patients with or without AAA diagnosis and used multivariate Cox regression model to evaluate mortality in patients with a positive AAA diagnosis adjusting for patient characteristics and comorbidities.
Results: We identified 3.9 million veterans with abdominal imaging, a total of 303,664 of whom were coded has having an AAA US screening between 2007 and 2018. An AAA diagnosis was made in 4.84% of the screening group vs. 1.3% in the non-screening imaging group P<0.001, yet more aneurysms were found with general imaging studies (50,730 vs.15,449) (Fig 1).
On Kaplan-Meier survival analysis, patients with an AAA diagnosis had higher overall mortality than patients who screened normal; patients with aneurysms found with non-screening imaging had the highest mortality, log-rank P<0.001 (Fig 2).
The difference in differences regression analysis, showed that the absolute AAA detection rate was 1.55% higher (95% CI 1.2- 1.8), and the mortality was 13.89 % lower (95% CI 10.18 %-16.66 %) after the introduction of the screening program in 2007.
Multivariate Cox regression analysis in patients with AAA diagnosis (65-74-year-old) demonstrated a significantly lower 5-year mortality [HR 0.45 (95% CI 0.43-0.48)] for patients in the US Screening group P<0.001.
Conclusions: In a nationwide analysis of VA patients, implementation of AAA screening was associated with improved survival and a higher rate of AAA diagnosis. These findings provide further support for this program’s continuation versus defaulting to incidental recognition following other abdominal imaging.
ABOUT MANUEL GARCIA-TOCA
Dr. Garcia-Toca earned his medical degree at the Universidad Anahuac in Mexico 1999. He has a master’s degree in Health Policy from Stanford University.
He received his general surgery training at the Massachusetts General Hospital and Brown University in 2008. He then completed a Vascular Surgery fellowship at Northwestern University in 2010. Dr. Garcia-Toca is board certified in both surgery and vascular surgery.
Dr. Garcia-Toca joined Stanford Vascular Surgery in 2015. He is currently Clinical Professor of Surgery in the Division of Vascular Surgery. Dr. Garcia-Toca had previously served as an Assistant Professor of Surgery at Brown University. Dr. Garcia Toca is a Staff Surgeon at Santa Clara Valley Medical Center in San Jose.
His research interests include new therapeutic strategies and outcomes for the management of vascular trauma, cerebrovascular diseases, dialysis access, aortic dissection and aneurysms.
ABOUT OLIVER O. AALAMI
Dr. Aalami is a Clinical Associate Professor of Vascular & Endovascular Surgery at Stanford University and the Palo Alto VA and serves as the Lead Director of Stanford’s Biodesign for Digital Health. He is the course director for Biodesign for Digital Health, Building for Digital Health and co-founder of the open source project, CardinalKit, developed to support sensor-based mobile research projects. His primary research focuses on clinically validating the sensors in smartphones and smartwatches in patients with cardiovascular disease to further precision health implementation.
Hosted by: Garry Gold, M.D.
Sponsored by the PHIND Center and the Department of Radiology