

Geert Litjens, PhD
Assistant Professor in Computational Pathology
Department of Pathology
Radboud University Medical Center
Title: Going Beyond What is Humanly Possible: Machine Learning for Clinical Pathology
Abstract: Machine learning advances in the past decade have revolutionized computer vision, and have since also made their way into medical imaging. Although many associate medical imaging with radiology first, clinical pathology might be more significantly impacted, at least in the short term by machine learning. Partly due to the simultaneous advent of machine learning in medicine and digital pathology, but perhaps mostly because in pathology achieving inhuman feats is surprisingly low-hanging fruit. In this presentation, I will give some examples analog to radiology, then illustrate some superhuman applications. Subsequently, I will highlight our current limitations and possible future research directions.
Radiology Department-Wide Research Meeting
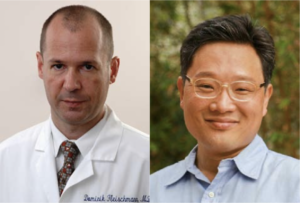
• Dominik Fleischmann, MD: 3DQ Lab Overview
• Tom Soh, PhD: Research Updates
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

Join us for the annual Precision Health & Integrated Diagnostics Symposium. This all-day virtual event will showcase the exciting PHIND work that is going on campus wide. The featured presentations will be from current PHIND investigators and Precision Health experts. We hope you can join us and look forward to building the PHIND community together.
The agenda and speaker information are available on the PHIND website. The event is fully virtual and the livestream link will be posted on the PHIND website closer to the event.

MIPS Seminar Series: “Circulating Tumor DNA Biomarkers for Therapy Monitoring and Early Detection”
Shan X. Wang, PhD
Leland T. Edwards Professor in the School of Engineering
Professor of Materials Science & Engineering, jointly of Electrical Engineering, and by courtesy of Radiology (Stanford School of Medicine)
Director, Stanford Center for Magnetic Nanotechnology
Stanford University
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/93202777468
Dial: +1 650 724 9799 or +1 833 302 1536
Webinar ID: 932 0277 7468
Passcode: 851144
12:00pm – 12:45pm Seminar & Discussion
RSVP Here
ABSTRACT
Inspired by Dr Sam Gambhir, MIPS, Canary Center, and Stanford CCNE have pursued in vivo imaging and in vitro diagnostic tests for cancer therapeutic response or early detection, respectively, over the last 15+ years. Here I present two successful examples based on circulating tumor DNA (ctDNA) targets in plasma, complementary to imaging modalities such as CT and Ultrasound.
We have developed a simple yet highly sensitive assay for the detection of actionable mutational targets such as Epidermal Growth Factor Receptor (EGFR) and Kirsten rat sarcoma oncogene (KRAS) mutations in the plasma ctDNA from non-small cell lung cancer (NSCLC) patients using giant magnetoresistive (GMR) nanosensors. Our assay achieves lower limits of detection compared to standard fluorescent PCR based assays, and comparable performance to digital PCR methods. In 30 patients with metastatic disease and known EGFR mutation status at diagnosis, our assay achieved 87.5% sensitivity for Exon19 deletion and 90% sensitivity for L858R mutation while retaining 100% specificity; additionally, our assay detected secondary T790M mutation resistance with 96.3% specificity while retaining 100% sensitivity. We re-sampled 13 patients undergoing tyrosine kinase inhibitor (TKI) therapy 2 weeks after initiation to assess response, our GMR assay was 100% accurate in correlation with longitudinal clinical outcome, and the responders identified by the GMR assay had significantly improved progression free survival (PFS) compared to the non-responders. The GMR assay is low cost, rapid, and portable, making it ideal for detecting actionable mutations at diagnosis and non-invasively monitoring treatment response in the clinic.
On another front, we have also developed a highly sensitive and multiplexed assay for the detection of methylated ctDNA targets in plasma samples. Current diagnostic tests for liver cancer in at-risk patients are cumbersome, costly and inaccurate, resulting in a need for accurate blood-based tests. By devising a Layered Analysis of Methylated Biomarkers (LAMB) from the relevant big data, we have discovered a set of DNA targets in the blood that accurately detects liver cancer in these at-risk patients. This set of methylated targets was found by analyzing the genetic information of 3411 liver cancer patients and 1722 healthy people. Our results could lead to clinical adoption of liquid biopsy tests for liver cancer surveillance in high-risk populations and the development of blood tests for other cancers.
ABOUT
Prof. Wang directs the Center for Magnetic Nanotechnology and is a leading expert in biosensors, information storage and spintronics. His research and inventions span across a variety of areas including magnetic biochips, in vitro diagnostics, cancer biomarkers, magnetic nanoparticles, magnetic sensors, magnetoresistive random access memory, and magnetic integrated inductors. He has over 300 publications, and holds 65 issued or pending patents in these and interdisciplinary areas. He was named an inaugural Fred Terman Fellow, and was elected a Fellow of the Institute of Electrical and Electronics Engineers (IEEE) and a Fellow of American Physical Society (APS) for his seminal contributions to magnetic materials and nanosensors. His team won the Grand Challenge Exploration Award from Gates Foundation (2010), the XCHALLENGE Distinguished Award (2014), and the Bold Epic Innovator Award from the XPRIZE Foundation (2017).
Dr. Wang cofounded three high-tech startups in Silicon Valley, including MagArray, Inc. and Flux Biosciences, Inc. In 2018 MagArray launched a first of its kind lung cancer early diagnostic assay based on protein cancer biomarkers and support vector machine (SVM). In 2019, Flux Biosciences launched a human trial to offer at-home testing of fertility based on hormones and magneto-nanosensors. Through his participation in the Center for Cancer Nanotechnology Excellence (as co-PI of the CCNE) and the Joint University Microelectronics Program (JUMP), he is actively engaged in the transformative research of healthcare and is developing emerging memories for energy efficient computing.
Hosted by: Katherine Ferrara, PhD
Sponsored by: Molecular Imaging Program at Stanford & the Department of Radiology

Mixed Reality for Surgical Guidance will take place on Thursday, April 1st from 9:00 – 10:30 am PDT.
The event will start with a one-hour panel discussion featuring Dr. Bruce Daniel of Stanford Radiology and the Stanford IMMERS Lab; Christoffer Hamilton of Brainlab, a surgical software and hardware leader in Germany; and Dr. Thomas Grégory of Orthopedic Surgery at the Université Sorbonne Paris Nord.
This panel will be moderated by Dr. Christoph Leuze of Stanford University and the Stanford Medical Mixed Reality (SMMR) program.
Immediately following the panel discussion, you are also invited to a 30-minute interactive session with the panelists where questions and ideas can be explored in real time.
Register here: https://stanford.zoom.us/meeting/register/tJcqf-GrqToiHNKL4D-5haRLowQylIwMEAve

Date: April 10, 2021 (8 AM-6PM)
-
- 8 AM-8:20 AM opening remarks Zainub and Pete
- 8:20 AM-9:20 AM Talk 1 “I fought the law and no one won”
- 10 minute Break
- 9:30 AM-10:30 AM talk 2 students and doctors with disabilities panel
- 20 minute break
-
- 10:50 AM-11:50 AM Breakout
- One hour lunch (TBD)
- 12:50 PM-1:50 PM Talk 3 the frontiers of disability research
- Lisa Meeks is moderating
- Bonnie Swenor invited
- 10 minute break
- 2:00 PM-3:00 PM breakout 2
- 10 minute break
- 3:10 PM-4:10 PM talk 4 do-it-yourself disability advocacy (Poullos/Tolchin with students)
- 4:10 PM-4:30 PM closing remarks
- 4:30 PM-6 PM virtual happy hour

Radiology Department-Wide Research Meeting
• Research Announcements
• Michelle James, PhD – Detecting and Tracking Immune Responses in the Brain and Beyond using PET
• Ryan Spitler, PhD – Precision Health and Integrated Diagnostics (PHIND) Center
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

PHIND Seminar Series: Impact of the Veterans Affairs National Abdominal Aortic Screening Program
Manuel Garcia-Toca, M.D.
Clinical Professor of Surgery
Chief, Division of Vascular Surgery
Santa Clara Valley Medical Center (SCVMC)
Oliver O. Aalami, M.D.
Clinical Associate Professor of Surgery, Vascular Surgery
Lucile Packard Children’s Hospital
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/98417624095
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Webinar ID: 984 1762 4095
Passcode: 111283
11:00am – 12:00pm Seminar & Discussion
RSVP Here
ABSTRACT
Background: The U.S. Federal Government enacted the Screen for Abdominal Aortic Aneurysms Very Efficiently Act in January 2007. Simultaneously, the Department of Veterans Affairs (VA) implemented a more inclusive AAA screening policy for veteran beneficiaries shortly afterwards.
Our study aimed to evaluate the impact of the VA program on AAA detection rate and all-cause mortality compared to a cohort of patients whose aneurysms were identified by other abdominal imaging.
Methods: We identified veterans with an AAA screening study using the two existing Current Procedural Terminology (CPT) codes (G0389 and 76706). In the comparison group, eligible abdominal imaging studies included ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) queried according to CPT codes between 2001 and 2018.
We used a difference-in-differences regression model to evaluate the change in aneurysm detection rate and all-cause mortality five years before and eleven years after the VA implemented the screening policy in 2007.
We calculated survival estimates after AAA screening or non-screening imaging of patients with or without AAA diagnosis and used multivariate Cox regression model to evaluate mortality in patients with a positive AAA diagnosis adjusting for patient characteristics and comorbidities.
Results: We identified 3.9 million veterans with abdominal imaging, a total of 303,664 of whom were coded has having an AAA US screening between 2007 and 2018. An AAA diagnosis was made in 4.84% of the screening group vs. 1.3% in the non-screening imaging group P<0.001, yet more aneurysms were found with general imaging studies (50,730 vs.15,449) (Fig 1).
On Kaplan-Meier survival analysis, patients with an AAA diagnosis had higher overall mortality than patients who screened normal; patients with aneurysms found with non-screening imaging had the highest mortality, log-rank P<0.001 (Fig 2).
The difference in differences regression analysis, showed that the absolute AAA detection rate was 1.55% higher (95% CI 1.2- 1.8), and the mortality was 13.89 % lower (95% CI 10.18 %-16.66 %) after the introduction of the screening program in 2007.
Multivariate Cox regression analysis in patients with AAA diagnosis (65-74-year-old) demonstrated a significantly lower 5-year mortality [HR 0.45 (95% CI 0.43-0.48)] for patients in the US Screening group P<0.001.
Conclusions: In a nationwide analysis of VA patients, implementation of AAA screening was associated with improved survival and a higher rate of AAA diagnosis. These findings provide further support for this program’s continuation versus defaulting to incidental recognition following other abdominal imaging.
ABOUT MANUEL GARCIA-TOCA
Dr. Garcia-Toca earned his medical degree at the Universidad Anahuac in Mexico 1999. He has a master’s degree in Health Policy from Stanford University.
He received his general surgery training at the Massachusetts General Hospital and Brown University in 2008. He then completed a Vascular Surgery fellowship at Northwestern University in 2010. Dr. Garcia-Toca is board certified in both surgery and vascular surgery.
Dr. Garcia-Toca joined Stanford Vascular Surgery in 2015. He is currently Clinical Professor of Surgery in the Division of Vascular Surgery. Dr. Garcia-Toca had previously served as an Assistant Professor of Surgery at Brown University. Dr. Garcia Toca is a Staff Surgeon at Santa Clara Valley Medical Center in San Jose.
His research interests include new therapeutic strategies and outcomes for the management of vascular trauma, cerebrovascular diseases, dialysis access, aortic dissection and aneurysms.
ABOUT OLIVER O. AALAMI
Dr. Aalami is a Clinical Associate Professor of Vascular & Endovascular Surgery at Stanford University and the Palo Alto VA and serves as the Lead Director of Stanford’s Biodesign for Digital Health. He is the course director for Biodesign for Digital Health, Building for Digital Health and co-founder of the open source project, CardinalKit, developed to support sensor-based mobile research projects. His primary research focuses on clinically validating the sensors in smartphones and smartwatches in patients with cardiovascular disease to further precision health implementation.
Hosted by: Garry Gold, M.D.
Sponsored by the PHIND Center and the Department of Radiology


Imon Banerjee, PhD
Assistant Professor
Co-director Medical and Health Informatics Core (MHIC)
Department of Biomedical Informatics
Department of Radiology
Member of Winship Cancer Institute
Emory School of Medicine
Fusion of Multi-Modal Data Stream for Clinical Event Prediction – Simulating Physicians’ Workflow
Abstract:
Advancements in machine learning and deep learning techniques carry the potential to make significant contributions to healthcare, particularly in fields of diagnosis, prognosis, and treatment decisions. However, most of current state-of-the-art machine learning and deep learning models for healthcare applications consider only a single input data stream without data informing clinical context. The trend of ignoring clinical contextual information is particularly prominent when dealing with the diagnosis and prognosis tasks where the imaging data is accessible. Yet in practice, pertinent and accurate non-imaging data based on the clinical history and laboratory data enable physicians to interpret imaging findings in the appropriate clinical context, leading to a higher diagnostic accuracy, informative clinical decision making, and improved patient outcomes. To achieve a similar goal using machine learning and increase the physician trust, clinical diagnosis and prognosis models must also achieve the capability to process contextual clinical data from electronic health records (EHR) in addition to pixel or other sensor data. This talk will present multiple fusion machine learning models on the imaging data with boosted performance by integrating the clinical context. In addition to imaging, I will also present a smart flexible sensor patch with on-chip AI capability that can be used in homecare to generate advance alert of cardiovascular abnormality by combining physiological signal data with patient demographic and comorbidity information.

MIPS Seminar Series: Emerging nanophotonic platforms for infectious disease diagnostics: Re-imagining the conventional microbiology toolkit
Jennifer Dionne, PhD
Senior Associate Vice Provost for Research Platforms/Shared Facilities
Associate Professor of Material Science and Engineering and, by courtesy, of Radiology (Molecular Imaging Program at Stanford)
Stanford University
Location: Zoom
Webinar URL: https://stanford.zoom.us/j/95883654314
Dial: +1 650 724 9799 or +1 833 302 1536
Webinar ID: 958 8365 4314
Passcode: 105586
12:00pm – 12:45pm Seminar & Discussion
RSVP Here
ABSTRACT
We present our research controlling light at the nanoscale for infectious disease diagnostics, including detecting bacteria at low concentration, sensing COVID gene sequences, and visualizing in-vivo inter-cellular forces. First, we combine Raman spectroscopy and deep learning to accurately classify bacteria by both species and antibiotic resistance in a single step. We design a convolutional neural network (CNN) for spectral data and train it to identify 30 of the most common bacterial strains from single-cell Raman spectra, achieving antibiotic treatment identification accuracies exceeding 99% and species identification accuracies similar to leading mass spectrometry identification techniques. Our combined Raman-CNN system represents a proof-of-concept for rapid, culture-free identification of bacterial isolates and antibiotic resistance. Second, we describe resonant nanophotonic surfaces, known as “metasurfaces” that enable multiplexed detection of SARS-CoV-2 gene sequences. Our metasurfaces utilize guided mode resonances excited in high refractive index nanostructures. The high quality factor modes produce a large amplification of the electromagnetic field near the nanostructures that increase the response to targeted binding of nucleic acids; simultaneously, the optical signal is beam-steered for multiplexed detection. We describe how this platform can be manufactured at scale for portable, low-cost assays. Finally, we introduce a new class of in vivo optical probes to monitor biological forces with high spatial resolution. Our design is based on upconverting nanoparticles that, when excited in the near-infrared, emit light of a different color and intensity in response to nano-to-microNewton forces. The nanoparticles are sub-30nm in size, do not bleach or photoblink, and can enable deep tissue imaging with minimal tissue autofluorescence. We present the design, synthesis, and characterization of these nanoparticles both in vitro and in vivo, focusing on the forces generated by the roundworm C. elegans as it feeds and digests its bacterial food.
ABOUT
Jennifer Dionne is the Senior Associate Vice Provost of Research Platforms/Shared Facilities and an associate professor of Materials Science and Engineering and, by courtesy, of Radiology at Stanford. She is also an Associate Editor of Nano Letters, director of the DOE-funded Photonics at Thermodynamic Limits Energy Frontier Research Center, and an affiliate faculty of the Wu Tsai Neurosciences Institute, the Institute for Immunity, Transplantation, and Infection, and Bio-X. Jen received her B.S. degrees in Physics and Systems Science and Mathematics from Washington University in St. Louis, her Ph. D. in Applied Physics at the California Institute of Technology in 2009, and her postdoctoral training in Chemistry at Berkeley. Her research develops nanophotonic methods to observe and control chemical and biological processes as they unfold with nanometer scale resolution, emphasizing critical challenges in global health and sustainability. Her work has been recognized with the Alan T. Waterman Award, a NIH Director’s New Innovator Award, a Moore Inventor Fellowship, the Materials Research Society Young Investigator Award, and the Presidential Early Career Award for Scientists and Engineers, and was featured on Oprah’s list of “50 Things that will make you say ‘Wow’!”. Beyond the lab, Jen enjoys exploring the intersection of art and science, long-distance cycling, and reliving her childhood with her two young sons.
Hosted by: Katherine Ferrara, PhD
Sponsored by: Molecular Imaging Program at Stanford & the Department of Radiology