
Radiology Department-Wide Research Meeting
• Curt Langlotz, MD, PhD: Overview of the AIMI Center
• Brian Hargreaves, PhD: Research Details from Town Hall, Q&A, and COVID19 Updates
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

CEDSS: Systematic identification of fluid-based biomarkers for ovarian and prostate cancer
Thomas Kislinger, Ph.D.
Professor & Chair
Department of Medical Biophysics
University of Toronto
Senior Scientist
Princess Margaret Cancer Centre
Zoom Webinar Details
Meeting URL: https://stanford.zoom.us/s/94878578384
Dial: +1 650 724 9799 or +1 833 302 1536
Webinar ID: 948 7857 8384
Passcode: 692692
Register Here
ABOUT
Thomas Kislinger received his MSc in Analytical Chemistry from the University of Munich, Germany (1998). He completed his PhD in 2001, investigating the role of Advanced Glycation Endproducts in diabetic vascular complications at the University of Erlangen, Germany and Columbia University, New York. Between 2002 and 2006 he completed a post-doctoral fellowship at the University of Toronto. In 2006 he joined the Princess Margaret Cancer Centre as an independent investigator. Dr. Kislinger holds positions as Senior Scientist at the Princess Margaret Cancer Centre and as Professor and Chair at the University of Toronto in the Department of Medical Biophysics. The Kislinger lab applies proteomics technologies to translational and basic cancer biology. This includes the development of novel proteomics methodologies, identification of liquid biopsy signatures and the molecular identification of novel cell surface markers.
Hosted by: Utkan Demirci, Ph.D.
Sponsored by: The Canary Center & the Department of Radiology
Stanford University – School of Medicine

PHIND Seminar Series: Maternal Trauma History, Attachment Style, and Depression Are Associated with Broad DNA Methylation Signatures in Infants
Thalia Robakis, M.D., Ph.D.
Associate Professor
Department of Psychiatry
Mount Sinai School of Medicine
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/95483174518
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Webinar ID: 954 8317 4518
Passcode: 179384
11:00am – 12:00pm Seminar & Discussion
RSVP Here
ABSTRACT
Background: The early environment provides many cues to young organisms that guide their development as they mature. Maternal personality and behavior are an important aspect of the environment of the developing human infant. The molecular mechanisms by which these influences are exerted are not well understood. We attempted to identify whether maternal traits could be associated with alterations in DNA methylation patterns in infants.
Methods: 32 women oversampled for history of depression were recruited in pregnancy and provided information on depressive symptoms, attachment style, and history of early life adversity. Buccal cell DNA was obtained from their infants at six months of age for a large-scale analysis of methylation patterns across 5×106 individual CpG dinucleotides, using clustering-based criteria for significance to control for multiple comparisons. Separately, associations between maternal depression, attachment style, and history of adversity and psychobehavioral outcomes in preschool-age children were examined.
Results: Tens of thousands of individual infant CpGs were alternatively methylated in association with each of the three studied maternal traits. Genes implicated in cell-cell communication, developmental patterning, growth, immune function/inflammatory response, and neurotransmission were identified. The result sets were highly coextensive among the three maternal traits, but areas of divergence exhibited intriguing parallels with behavioral outcomes.
Conclusions: Maternal personality traits are an important aspect of the infant environment that shapes offspring development in many ways. Infant genes that are epigenetically modified in reponse to maternal traits are potential candidate mediators for these effects. We have identified a large number of such genes and demonstrated parallels to clinically measurable outcomes in children.
ABOUT
Dr. Robakis is a psychiatrist with clinical and research interests in perinatal mood disorders and in the contribution of early life experiences to adult mental health and illness. She completed her M.D. as well as a Ph.D. in developmental neurobiology at Columbia University’s Medical Scientist Training Program, residency training in psychiatry at Stanford University School of Medicine, and a research fellowship in perinatal mood disorders also at Stanford. She remained on the clinical faculty at Stanford until 2019, when she accepted a position at the Icahn School of Medicine at Mount Sinai, where she is currently Associate Clinical Professor of Psychiatry and Assistant Director of the Women’s Mental Health Program.
Dr. Robakis’ research interests include the effects of early life stress and disordered attachment on risk for psychiatric illness in the perinatal period, on alterations in metabolism and cognition, and on psychobehavioral development in offspring. She is particularly interested in using epigenetic marks to help identify the biological pathways through which early life experiences exert their effects on outcomes in adulthood and intergenerationally.
Hosted by: Garry Gold, M.D.
Sponsored by the PHIND Center and the Department of Radiology

Radiology Department-Wide Research Meeting
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
February 19 Speakers:
Bruce Daniel, MD – Center Overview: IMMERS
Jennifer McNab, PhD – Encoding and Decoding Diffusion MRI
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

CEDSS: Disseminated cell hybrids as biomarkers for cancer detection, prognosis and treatment response
Melissa Wong, Ph.D.
Associate Professor and Vice Chair
Department of Cell, Development and Cancer Biology
Program Co-Lead, Knight Cancer Institute
Oregon Health & Science University
Zoom Details
Meeting URL: https://stanford.zoom.us/s/98184098662
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Meeting ID: 981 8409 8662
Passcode: 084321
ABSTRACT
Metastatic progression defines the final stages of tumor evolution and underlies the majority of cancer-related deaths. The heterogeneity in disseminated tumor cell populations capable of seeding and growing in distant organ sites contributes to the development of treatment resistant disease. We recently reported the identification of a novel tumor-derived cell population, circulating hybrid cells (CHCs), harboring attributes from both macrophages and neoplastic cells, including functional characteristics important to metastatic spread. These disseminated hybrids outnumber conventionally defined circulating tumor cells (CTCs) in cancer patients. It is unknown if CHCs represent a generalized cancer mechanism for cell dissemination, or if this population is relevant to the metastatic cascade. We detect CHCs in the peripheral blood of patients with cancer in myriad disease sites encompassing epithelial and non-epithelial malignancies. Further, we demonstrate that in vivo-derived hybrid cells harbor tumor-initiating capacity in murine cancer models and that CHCs from human breast cancer patients express stem cell antigens, features consistent with the ability to seed and grow at metastatic sites. We reveal heterogeneity of CHC phenotypes reflect key tumor features, including oncogenic mutations and functional protein expression. Importantly, this novel population of disseminated neoplastic cells opens a new area in cancer biology and renewed opportunity for battling metastatic disease.
ABOUT
The research focus of the Wong laboratory revolves around understanding the regulatory mechanisms that control epithelial stem cell homeostasis and their expansion in developmental, homeostasis and disease contexts, including cancer. I have substantial training and experience in intestinal stem cell investigation leveraging in vivo and ex vivo modeling, as well as in myriad cutting edge technologies (i.e. cyCIF, scRNA-seq). My publication record spans my post-doctoral fellowship in Dr. Jeffrey Gordon’s laboratory at Washington University School of Medicine, to studies in my own laboratory at Oregon Health & Science University. Our research impacts the understanding of regulatory mechanisms that govern cell state in the context of the evolving tissue microenvironment and changing cell signaling landscape, in development and disease.
Our studies in stem cell regulation led to the intriguing finding that stem cells can fuse with tissue macrophages in the context of injury repair and may impact tissue regeneration. We have extended these findings to the cancer setting, where cancer-macrophage fusions are detectible in primary and metastatic tumors, and my group recently identified and characterized these cells as a novel circulating tumor cell population. Importantly, our studies in cell culture, in mice and humans provide an indepth evaluation of hybrid cells to set the foundation for continued investigations into their biology, impact on disease progression or tissue regeneration, and use as a biomarker for disease burden. Importantly, we coined the term, circulating hybrid cell (CHC) for this novel population and reported they exist at higher levels than conventionally defined circulating tumor cells in the peripheral blood of cancer patients. This work was published in 2018 and highlighted by Science Magazine as one of the top ten publications in the cancer field in the science family journals. The science proposed in this U01 application leverage hybrid cell biology to assess treatment response and resistance in breast cancer patients undergoing targeted therapy. Our proposal leverages active collaborations with Dr. Young Hwan Young’s group to synergize biology with computation, as well as a number of other valuable collaborators to ensure success of the proposed, cutting-edge science.
Hosted by: Utkan Demirci, Ph.D.
Sponsored by: The Canary Center & the Department of Radiology
Stanford University – School of Medicine
Radiology Department-Wide Research Meeting
• Dominik Fleischmann, MD: 3DQ Lab Overview
• Tom Soh, PhD: Research Updates
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

Radiology Department-Wide Research Meeting
• Research Announcements
• Michelle James, PhD – Detecting and Tracking Immune Responses in the Brain and Beyond using PET
• Ryan Spitler, PhD – Precision Health and Integrated Diagnostics (PHIND) Center
Location: Zoom – Details can be found here: https://radresearch.stanford.edu
Meetings will be the 3rd Friday of each month.
Hosted by: Brian Hargreaves, PhD
Sponsored by: the the Department of Radiology

PHIND Seminar Series: Impact of the Veterans Affairs National Abdominal Aortic Screening Program
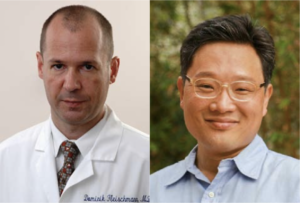
Manuel Garcia-Toca, M.D.
Clinical Professor of Surgery
Chief, Division of Vascular Surgery
Santa Clara Valley Medical Center (SCVMC)
Oliver O. Aalami, M.D.
Clinical Associate Professor of Surgery, Vascular Surgery
Lucile Packard Children’s Hospital
Location: Zoom
Webinar URL: https://stanford.zoom.us/s/98417624095
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Webinar ID: 984 1762 4095
Passcode: 111283
11:00am – 12:00pm Seminar & Discussion
RSVP Here
ABSTRACT
Background: The U.S. Federal Government enacted the Screen for Abdominal Aortic Aneurysms Very Efficiently Act in January 2007. Simultaneously, the Department of Veterans Affairs (VA) implemented a more inclusive AAA screening policy for veteran beneficiaries shortly afterwards.
Our study aimed to evaluate the impact of the VA program on AAA detection rate and all-cause mortality compared to a cohort of patients whose aneurysms were identified by other abdominal imaging.
Methods: We identified veterans with an AAA screening study using the two existing Current Procedural Terminology (CPT) codes (G0389 and 76706). In the comparison group, eligible abdominal imaging studies included ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) queried according to CPT codes between 2001 and 2018.
We used a difference-in-differences regression model to evaluate the change in aneurysm detection rate and all-cause mortality five years before and eleven years after the VA implemented the screening policy in 2007.
We calculated survival estimates after AAA screening or non-screening imaging of patients with or without AAA diagnosis and used multivariate Cox regression model to evaluate mortality in patients with a positive AAA diagnosis adjusting for patient characteristics and comorbidities.
Results: We identified 3.9 million veterans with abdominal imaging, a total of 303,664 of whom were coded has having an AAA US screening between 2007 and 2018. An AAA diagnosis was made in 4.84% of the screening group vs. 1.3% in the non-screening imaging group P<0.001, yet more aneurysms were found with general imaging studies (50,730 vs.15,449) (Fig 1).
On Kaplan-Meier survival analysis, patients with an AAA diagnosis had higher overall mortality than patients who screened normal; patients with aneurysms found with non-screening imaging had the highest mortality, log-rank P<0.001 (Fig 2).
The difference in differences regression analysis, showed that the absolute AAA detection rate was 1.55% higher (95% CI 1.2- 1.8), and the mortality was 13.89 % lower (95% CI 10.18 %-16.66 %) after the introduction of the screening program in 2007.
Multivariate Cox regression analysis in patients with AAA diagnosis (65-74-year-old) demonstrated a significantly lower 5-year mortality [HR 0.45 (95% CI 0.43-0.48)] for patients in the US Screening group P<0.001.
Conclusions: In a nationwide analysis of VA patients, implementation of AAA screening was associated with improved survival and a higher rate of AAA diagnosis. These findings provide further support for this program’s continuation versus defaulting to incidental recognition following other abdominal imaging.
ABOUT MANUEL GARCIA-TOCA
Dr. Garcia-Toca earned his medical degree at the Universidad Anahuac in Mexico 1999. He has a master’s degree in Health Policy from Stanford University.
He received his general surgery training at the Massachusetts General Hospital and Brown University in 2008. He then completed a Vascular Surgery fellowship at Northwestern University in 2010. Dr. Garcia-Toca is board certified in both surgery and vascular surgery.
Dr. Garcia-Toca joined Stanford Vascular Surgery in 2015. He is currently Clinical Professor of Surgery in the Division of Vascular Surgery. Dr. Garcia-Toca had previously served as an Assistant Professor of Surgery at Brown University. Dr. Garcia Toca is a Staff Surgeon at Santa Clara Valley Medical Center in San Jose.
His research interests include new therapeutic strategies and outcomes for the management of vascular trauma, cerebrovascular diseases, dialysis access, aortic dissection and aneurysms.
ABOUT OLIVER O. AALAMI
Dr. Aalami is a Clinical Associate Professor of Vascular & Endovascular Surgery at Stanford University and the Palo Alto VA and serves as the Lead Director of Stanford’s Biodesign for Digital Health. He is the course director for Biodesign for Digital Health, Building for Digital Health and co-founder of the open source project, CardinalKit, developed to support sensor-based mobile research projects. His primary research focuses on clinically validating the sensors in smartphones and smartwatches in patients with cardiovascular disease to further precision health implementation.
Hosted by: Garry Gold, M.D.
Sponsored by the PHIND Center and the Department of Radiology

Targeted violence continues against Black Americans, Asian Americans, and all people of color. The department of radiology diversity committee is running a racial equity challenge to raise awareness of systemic racism, implicit bias and related issues. Participants will be provided a list of resources on these topics such as articles, podcasts, videos, etc., from which they can choose, with the “challenge” of engaging with one to three media sources prior to our session (some videos are as short as a few minutes). Participants will meet in small-group breakout sessions to discuss what they’ve learned and share ideas.
Please reach out to Marta Flory, flory@stanford.edu with questions. For details about the session, including recommended resources and the Zoom link, please reach out to Meke Faaoso at mfaaoso@stanford.edu.

CEDSS: “Building a Scalable Clinical Genomics Program: How tumor, normal, and plasma DNA sequencing are informing cancer care, cancer risk, and cancer detection”
Elizabeth and Felix Rohatyn Chair & Associate Director of the Marie-Josée and Henry R. Kravis Center for Molecular Oncology
Memorial Sloan Kettering Cancer Center
Zoom Details
Meeting URL: https://stanford.zoom.us/s/92559505314
Dial: US: +1 650 724 9799 or +1 833 302 1536 (Toll Free)
Meeting ID: 925 5950 5314
Passcode: 418727
11:00am – 12:00pm Seminar & Discussion
RSVP Here
ABSTRACT
Tumor molecular profiling is a fundamental component of precision oncology, enabling the identification of oncogenomic mutations that can be targeted therapeutically. To accelerate enrollment to clinical trials of molecularly targeted agents and guide treatment selection, we have established a center-wide, prospective clinical sequencing program at Memorial Sloan Kettering Cancer Center using a custom, paired tumor-blood normal sequencing assay (MSK-IMPACT), which we have used to profile more than 50,000 patients with solid tumors. Yet beyond just the characterization of tumor-specific alterations, the inclusion of blood DNA has readily enabled the identification of germline risk alleles and somatic mutations associated with clonal hematopoiesis. To complement this approach, we have also implemented a ‘liquid biopsy’ cfDNA panel (MSK-ACCESS) for cancer detection, surveillance, and treatment selection and monitoring. In my talk, I will describe the prevalence of somatic and germline genomic alterations in a real-world population, the clinical benefits of cfDNA assessment, and how clonal hematopoiesis can inform cancer risk and confound liquid biopsy approaches to cancer detection.
ABOUT
Michael Berger, PhD, holds the Elizabeth and Felix Rohatyn Chair and is Associate Director of the Marie-Josée and Henry R. Kravis Center for Molecular Oncology at Memorial Sloan Kettering Cancer Center, a multidisciplinary initiative to promote precision oncology through genomic analysis to guide the diagnosis and treatment of cancer patients. He is also an Associate Attending Geneticist in the Department of Pathology with expertise in cancer genomics, computational biology, and high-throughput DNA sequencing technology. His laboratory is developing experimental and computational methods to characterize the genetic makeup of individual cancers and identify genomic biomarkers of drug response and resistance. As Scientific Director of Clinical NGS in the Molecular Diagnostics Service, he oversees the development and bioinformatics associated with clinical sequencing assays, and he helped lead the development and implementation of MSK-IMPACT, a comprehensive FDA-authorized tumor sequencing panel that been used to profile more than 60,000 tumors from advanced cancer patients at MSK. The resulting data have enabled the characterization of somatic and germline biomarkers across many cancer types and the identification of mutations associated with clonal hematopoiesis. Dr. Berger also led the development of a clinically validated plasma cell-free DNA assay, MSK-ACCESS, which his laboratory is using to explore tumor evolution, acquired drug resistance, and occult metastatic disease. He received his Bachelor’s Degree in Physics from Princeton University and his Ph.D. in Biophysics from Harvard University.
Hosted by: Utkan Demirci, Ph.D.
Sponsored by: The Canary Center & the Department of Radiology
Stanford University – School of Medicine